Published: January 26, 2012

Flickr: By Pedro Moura Pinheiro
Pilot study suggests infrared analysis of white blood cells is a promising strategy for diagnosis of Alzheimer’s disease
Spanish researchers, led by Pedro Carmona from the Instituto de Estructura de la Materia in Madrid, have uncovered a new promising way to diagnose Alzheimer’s disease more accurately. Their technique, which is non-invasive, fast and low-cost, measures how much infrared radiation is either emitted or absorbed by white blood cells. Because of its high sensitivity, this method is able to distinguish between the different clinical stages of disease development thereby allowing reliable diagnosis of both mild and moderate stages of Alzheimer’s. The work is published online in Springer’s journal Analytical & Bioanalytical Chemistry. [continue reading…]
Published: January 4, 2012

istockphoto
he first changes in the brain of a person with Alzheimer’s disease can be observed as much as ten years in advance – ten years before the person in question has become so ill that he or she can be diagnosed with the disease. This is what a new study from
Lund University in Sweden has found.
Physician Oskar Hansson and his research group are studying biomarkers – substances present in spinal fluid and linked to Alzheimer’s disease. The group has studied close to 140 people with mild memory impairment, showing that a certain combination of markers (low levels of the substance beta-amyloid and high levels of the substance tau) indicate a high risk of developing Alzheimer’s disease in the future.
As many as 91 per cent of the patients with mild memory impairment who had these risk markers went on to develop Alzheimer’s within a ten-year period. In contrast, those who had memory impairment but normal values for the markers did not run a higher risk of getting Alzheimer’s than healthy individuals. [continue reading…]
Published: October 8, 2011

istockphoto
hile medical researchers continue the search for advanced diagnosis, prevention and treatment of dementia, a researcher at
Royal Holloway, University of London is focusing on improving the experiences of those already suffering with the devastating disease for whom any cure would be too late.
Professor Helen Nicholson is devoting her time to evaluating a pioneering project which enables advanced dementia sufferers to take part in art, drama and dance projects.
Hearts and Minds is a unique creative arts and reminiscence project, run by Age Exchange, specifically for older people with Alzheimer’s or other forms of dementia but also including people with other mental health needs such as schizophrenia and depression.
Artists are be working with care staff in South London and Maudsley NHS Trust to hold group work and one-to-one performing arts session with dementia sufferers.
Dementia is a terrifying and isolating disease that affects brain function and in particular the ability to remember, think and reason. Around 750,000 people have been diagnosed with dementia in the UK and the Department of Health predicts that this number is to double in the next 30 years. There is no cure and symptoms will get worse over time.
Although dementia sufferers often have little or no short term memory, their long term memory is intact and they can use this in the Hearts and Minds project. [continue reading…]
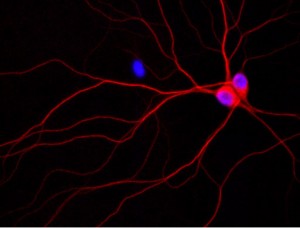
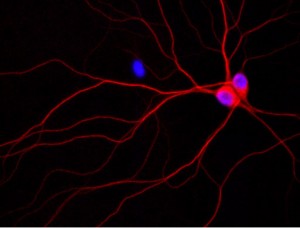
Image of rat neurons growing in a culture dish. The purple spheres are the cell nuclei and the red corresponds to the localization of phosphorylated tau.X Credit: Jack Reifert, U
In what they are calling a new direction in the study of Alzheimer’s disease, UC Santa Barbara scientists have made an important finding about what happens to brain cells that are destroyed in Alzheimer’s disease and related dementias. The results are published in the online version of The Journal of Biological Chemistry.
Stuart Feinstein, professor of Molecular, Cellular and Developmental Biology, senior author, and co-director of UCSB’s Neuroscience Research Institute, explained: “With dementia, the brain cells, or neurons, that you need for cognitive skills are no longer working properly. Then, they’re not even there anymore because they die. That’s what leads to dementia; you’re losing neuronal capacity.”
Feinstein has studied the protein called “tau” for about 30 years, using test tube biochemistry and a variety of cultured cells as models. Under normal conditions, tau is found in the long axons of neurons that serve to connect neurons with their targets, often far from the cell body itself. Among tau’s major functions is to stabilize microtubules, which are an integral part of the cellular cytoskeleton that is essential for many aspects of neuronal cell structure and function.
It has been known for many years that a small peptide named amyloid beta can cause neuronal cell death and Alzheimer’s disease, although the mechanism for how it works has been poorly understood. Recently, genetic evidence has demonstrated that the ability of amyloid beta to kill neurons requires tau; however, what it does to tau has been enigmatic. “We know amyloid beta is a bad guy,” said Feinstein. “Amyloid beta causes disease; amyloid beta causes Alzheimer’s. The question is how does it do it?” [continue reading…]