Published: November 23, 2010
Most patients who take anti-depressants give up their treatment in less than six months, the minimum period recommended for treating severe depression and other derived pathologies. This is the conclusion of a new study carried out by Catalan researchers, which reveals that only 25% continue their treatment for more than 11 months.
“Only one in every five patients properly completes their treatment”, Catalina Serna, co-author of the study, and an expert at the Jordi Gol Primary Care Research Institute (IDIAP) in Lleida, tells SINC. [continue reading…]
 Psychologist Irving Kirsh aims to “explode the myth” of Prozac and its ilk, arguing that there’s little evidence that they actually work for most patients.
Psychologist Irving Kirsh aims to “explode the myth” of Prozac and its ilk, arguing that there’s little evidence that they actually work for most patients.
The following article is a sample from DISCOVER’s special Brain issue, available only on newsstands through June 28.
Depression is a chemical imbalance, most people think. Researchers, drug manufacturers, and even the Food and Drug Administration assert that antidepressants work by “normalizing” levels of brain neurotransmitters—chemical messengers such as serotonin. And yet hard science supporting this idea is quite poor, says Irving Kirsch, professor of psychology at the University of Hull in the U.K. An expert on the placebo effect, Kirsch has unearthed evidence that antidepressants do not correct brain chemistry gone awry. More important, the drugs are not much more effective against depression than are sugar pills, he says. To support these controversial claims, Kirsch conducted a meta-analysis, digging up data from unpublished clinical trials. When all the evidence is weighed together, Prozac, Paxil, and other such popular pills seem to be at best weakly effective against depression—an argument Kirsch presses in his new book, The Emperor’s New Drugs. Some other research backs up his claims. A study published this winter in the Journal of the American Medical Association found that psychoactive drugs are no better than placebos for people suffering from mild to moderate depression. link to continue reading
Source: Discover
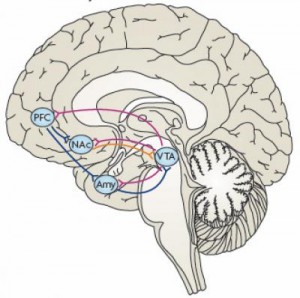
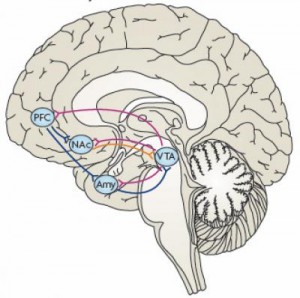
The transcription factor deltaFosB mediates resilience in the nucleus accumbens, hub of the brain’s reward circuit. It is the target of an intensive high tech screening for small molecules that tweak it, which could lead to a new class of resilience-boosting antidepressants.
cientists have discovered a mechanism that helps to explain resilience to stress, vulnerability to depression and how antidepressants work. The new findings, in the reward circuit of mouse and human brains, have spurred a high tech dragnet for compounds that boost the action of a key gene regulator there, called deltaFosB.
A molecular main power switch – called a transcription factor – inside neurons, deltaFosB turns multiple genes on and off, triggering the production of proteins that perform a cell’s activities.
“We found that triggering deltaFosB in the reward circuit’s hub is both necessary and sufficient for resilience; it protects mice from developing a depression-like syndrome following chronic social stress,” explained Eric Nestler, M.D., of the Mount Sinai School of Medicine, who led the research team, which was funded by the National Institute of Mental Health (NIMH). [continue reading…]
Published: October 5, 2009
The recent top 10 anti-depressants list is the most searched item currently on this blog. So the following should be of interest to many. Prospect magazine recently featured article The Drugs Don’t Work The article looks at Irvine Kirsch’s crusade to challenge the establishment by questioning whether anti-depressants are any better than placebo.
Kirsch has set out to challenge the antidepressant establishment. He claims that the SSRIs only appear to be effective because patients believe that they are going to work. “It’s placebo effect,” says Kirsch. In other words, the SSRIs are no better than blood-letting, snake oil, or any of the nostrums peddled before the era of modern medicine. Of course we all use placebos in everyday life, from kissing a child’s bruise better to taking a glass of brandy for a cold. I know a woman who saves red Smarties in a jar and takes one when she has a headache; she swears that it works even though she’s conscious that it’s placebo. Yet one would not want to build a health strategy for depression on such flimsy efficacy.
Source: Prospect